A STUDY ON RHEUMATOID ARTHRITIS: DIAGNOSIS AND TREATMENT USING CRP AND ESR MEASUREMENTS
Prepared by the researche
- Ghufran Younus Khairullah ALQARAGULI1: Al-Rifai Teaching Hospital
- Doaa kazem ghanem2: University of Sumer
Democratic Arabic Center
Journal of Progressive Medical Sciences : First issue – May 2025
A Periodical International Journal published by the “Democratic Arab Center” Germany – Berlin
R N/VIR. 3366 – 4508 .B
Journal of Progressive Medical Sciences
:To download the pdf version of the research papers, please visit the following link
Abstract
Rheumatoid arthritis (RA) is a chronic, progressive autoimmune disease characterized by systemic inflammation, synovial joint damage, and disability if left untreated. This study explores the etiopathogenesis, diagnostic criteria, and treatment strategies for RA, emphasizing the role of clinical and laboratory markers such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and rheumatoid factor (RF) in disease assessment.
The research highlights the multifactorial nature of RA, involving genetic predisposition (e.g., HLA-DRB1 alleles), environmental triggers (e.g., smoking, infections), and epigenetic modifications. Diagnostic adherence to the 2010 ACR/EULAR classification criteria—incorporating joint involvement, serology (RF/anti-CCP), and acute-phase reactants (ESR/CRP)—facilitates early intervention, crucial for preventing irreversible joint damage.
A cohort of 35 RA patients (23 females, 12 males; aged 30–70 years) was analyzed, revealing elevated ESR and CRP levels correlating with disease activity. Females exhibited higher susceptibility, aligning with global epidemiological trends. Treatment paradigms prioritize early, aggressive use of disease-modifying antirheumatic drugs (DMARDs), including conventional (e.g., methotrexate), targeted synthetic (JAK inhibitors), and biologic agents (TNF-α inhibitors), aiming for remission or low disease activity.
Key findings underscore the importance of: Early diagnosis via clinical-serological integration, Gender-specific considerations in RA management, Inflammatory markers (ESR/CRP) as prognostic tools, Personalized DMARD therapy to mitigate structural damage.
This study advocates standardized monitoring and tailored therapeutic strategies to improve outcomes in RA patients, addressing both articular and systemic manifestations.
INTRODUCTION:
Rheumatoid arthritis (RA) is a chronic, multi-system inflammatory autoimmune disease of indefinite etiology. The disease primarily affects synovial joints, eventually progressing to ongoing inflammation, destruction of both cartilaginous and bony elements of the joint, with resultant pain and disability. The disease additionally displays a spectrum of extra-articular multisystem manifestations (Smolen et al., 2016). The worldwide prevalence of RA remains underestimated. Data gathered from Western regions illustrated prevalence between 0.5 and 1% in white individuals, with prevalence rates ranging between 0.6 and 0.9% in the studied black individuals. The female to male ratio in rheumatoid arthritis is 2:1 to 3:1. A high concordance rate is observed in monozygotic twins, 12–15% compared to 2–3% in dizygotic twins (Malemba et al., 2012).
Theories behind the evolution of autoimmunity in rheumatoid arthritis are multifactorial. The inflammatory process usually develops in a predisposed individual who is probably exposed to a provocative trigger of autoimmunity via epigenetic modifications. Several risk factors, comprising genetic as well as non-genetic elements, provide a hostile environment for the change towards autoimmunity. Evidence revealed a significant impact of familial genetic risk factors, featuring ≥50% of the total risk of developing seropositive RA, with the highest incidence rates among first-degree relatives. Among the most influential non-genetic risk factors there comes smoking. Smoking provides a stimulus to epigenetic transformation, particularly in individuals with high-risk RA-susceptibility alleles.
Environmental risk factors also include; particulate exposure, periodontal disease, bronchiectasis, diet, obesity and the oral contraceptive impact, respiratory, oral, intestinal and genital tract mucosal sites (Malmström et al., 2017) , Figure 1.
Figure 1.
Etio-pathogenic factors and disease evolution in rheumatoid arthritis.
Neo-epitopes generation: genetic and environmental factors operate to ultimately result in the inflammatory and destructive synovial response. Stressors including cigarette smoke can act on cells in mucosal sites and promote post-translational conversion of the amino acid arginine to citrulline in a range of proteins, including intracellular proteins (such as histones) and matrix proteins (for example, fibronectin, collagen, fibrinogen, enolase and vimentin) via induction of peptidyl arginine diagnosis in a process called citrullination (also known as deamination) rendering them antigenic.
Citrullination may also be induced by the oral microbiota: P. gingivalis, common in periodontal disease, which expresses peptidyl arginine deiminases and can induce citrullination. A. actinomycetemcomitans, also producing a toxin that increases calcium influx into neutrophils, can lead to citrullination of peptides and has been recently implicated in RA etiology. Post-translational modifications (citrullination, carbamylating, and acetylation) can generate neo-epitopes (neo-peptide antigens). Animal and human data about autoimmunity in rheumatoid arthritis suggest a model in which multiple environmental influences affect mucosal immune function, promoting epigenetic transformations with trafficking of pro-inflammatory PAMPs, making use of the enhanced mucosal permeability. Hence, the initial shift towards autoimmunity may present at mucosal sites as reported in previous research with sputum samples positive for ACPA-IgA and IgG (Bodkhe et al., 2019).
Major histocompatibility complex binding and peptide presentation: specific class II human leukocyte antigen (HLA; also known as major histocompatibility complex—MHC) loci, which encode MHC molecules HLA-DRB1*01 and HLA-DRB1*04, display a very strong association with RA. The altered peptides bind to MHC protein heterodimers on antigen-presenting cells, especially those containing the shared epitope [a specific amino acid motif QKRAA commonly encoded by some alleles of the HLA-antigen D-related (DR) locus, significantly associated with the risk of developing RA].
Being bound to MHC complex, the antigenic epitope gets presented by the antigen-presenting cells (dendritic cells and macrophages) to the antigen-specific T lymphocyte receptor to stimulate T lymphocyte activation and differentiation. Over 100 non-HLA genetic risk factors (loci) including polymorphisms of PTPN22, TRAF1-C5, STAT4, TNFAIP3, and PADI4 have been associated with an increased risk of developing RA.
The adaptive immune system: the activated T lymphocyte stimulates the release of pro-inflammatory cytokines, including RANKL, TNF-α, GM-CSF, IL-2, IL-17, and IFN-γ. The antigen-stimulated T lymphocyte then promotes B cell priming via T-B cell receptor signaling pathways, then stimulates specific antibody responses by the stimulated B lymphocytes against the neo-epitopes (neo-antigens), promoting a self-directed immune response. In addition to autoantibody production, the activated B lymphocytes release IL-6 (Firestein & McInnes, 2017).
In situ activation of stromal cells: fibroblast-like synoviocytes FLS, antigen presenting cells and macrophages within the synovial joints gets similarly and synchronously stimulated to release a cascade of pro-inflammatory mediators promoting arthritis with cartilage and bone damage.
FLS master’s the intra-articular production of prodigious MMPs and small-molecule mediators such as MMPs, prostaglandins, leukotrienes, and RANKL. They additionally express IL-6 receptors and specific patterns of microRNAs that could contribute to their activated phenotype. FLS exhibits an invasive phenotype that is responsible for cartilage damage and can potentially migrate from the joint to propagate disease. The macrophages, like synoviocytes, participate actively via local release of TNF-α, IL-1, IL-6, IL-8, and chemokines (CCL19, CCL21) (Ferreira et al., 2013).
Ectopic germinal centers: the adaptive immune cells infiltrate the synovial sublining with almost half of the sublining cells CD4+ memory T cells that can either diffusely infiltrate the tissue or, in 15–20% of patients, form ectopic germinal centers in which mature B cells proliferate, differentiate and produce antibodies (rheumatoid factor RF and anti-citrullinated C peptide ACCP).
The development of manifest disease in rheumatoid susceptible patients usually requires a second hit driven by cross-reactivity, or molecular mimicry to pathogen-specific antigens, in the settings of an inevitable lag of pathogen-immune complex clearance (Figure 2).
Figure 2.
Proximal interphalangeal joint with macrophages, dendritic cells, T cells, B cells, infiltrate with hypertrophied synovium, intra-synovial angiomatoids, and pannus formation. “By Dr. Maya H Ibrahim,” the original image provider.
Clinically, RA patients typically present with a recent onset of tender and swollen joints, morning joint stiffness, generalized sickness symptoms, as well as abnormal laboratory tests. Timely and precise diagnosis is of high importance in RA treatment, since early diagnosis can arrest disease in many patients, thereby preventing or substantially slowing disease progression, irreparable joint damage, and disability in up to 90% of RA patients (Aletaha & Smolen, 2018). The diagnosis of rheumatoid arthritis requires the integration of proper history taking, careful clinical examination and investigations. Patients might face a period of delay in establishing their diagnosis from weeks to months due to incomplete or intermittent symptoms, defective/unaccomplished clinical/radiographic and laboratory assessments particularly with early disease and assessment of laboratory markers such as elevated levels of CRP and ESR in serum and detection of RA-specific autoantibodies (Villeneuve et al., 2013).
- Standard of care in rheumatoid arthritis aims at the following (Smolen et al., 2010) :
- Establishing early diagnosis of RA.
- Identifying arthritis in need of treatment.
- Designing the ideal way to successfully initiate synthetic non biologic DMARDS.
- Providing low remission rates with standard DMARDs.
- Identifying other potential therapeutic targets in aggressive disease.
- Ensuring availability and safety of biologic DMARDS.
- Providing standardized measures for patient assessment, follow-up and treatment modulation.
The recently adopted American College of Rheumatology/European League Against Rheumatism ACR/EULAR classification criteria were established in 2010 with the aim of identifying patients with early inflammatory arthritis that is mostly due to rheumatoid arthritis. They have been proposed by the faculty as classification rather than diagnostic criteria to facilitate stratifying patients with similar characteristics for clinical research studies, particularly clinical trials with intent to treat. The development of diagnostic criteria for RA, like other autoimmune disorders, is still challenged by inter-individual variability and the risk of misdiagnosis. However, the current criteria might be used to inform diagnostic decision-making in clinical practice (Aletaha et al., 2010).
Rheumatological tests are medical tests used to diagnose and monitor rheumatic diseases, which are conditions that affect the joints, bones, muscles, and other soft tissues. These tests can help doctors identify the underlying cause of symptoms, such as joint pain, stiffness, and swelling.
Some of the most common rheumatological tests include:
- Rheumatoid factor (RF) test: This blood test measures the level of RF antibodies in the blood. RF is often elevated in people with rheumatoid arthritis and other autoimmune diseases.
- Anti-cyclic citrullinated peptide (anti-CCP) antibody test: This blood test measures the level of anti-CCP antibodies in the blood. Anti-CCP antibodies are often elevated in people with rheumatoid arthritis.
- Erythrocyte sedimentation rate (ESR) test: This blood test measures the rate at which red blood cells settle to the bottom of a test tube over time. A high ESR rate may indicate inflammation in the body, which is often associated with rheumatic diseases.
- C-reactive protein (CRP) test: This blood test measures the level of CRP, a protein that is produced in response to inflammation. A high CRP level may indicate inflammation in the body, which is often associated with rheumatic diseases.
- Joint fluid analysis: This test involves removing a sample of fluid from a swollen joint and analyzing it for signs of inflammation or infection.
- X-rays and imaging tests: These tests can help doctors identify structural changes in the joints and soft tissues that may be associated with rheumatic diseases.
It’s important to note that rheumatological tests are not definitive and should be interpreted in the context of a person’s symptoms, medical history, and physical examination findings. A diagnosis of a rheumatic disease often involves a combination of tests and clinical judgment.
The classification criteria proposed by the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) included clinical and serological variables that can be applied only to individuals with ≥1 swollen joint (Aletaha et al., 2010).
Any swollen or tender joint (excluding the distal interphalangeal joints of hands and feet, the first metatarsophalangeal joints and the first carpometacarpal joints) on clinical examination; additional evidence from MRI or ultrasonography may be used to identify additional joints.
1- large joint (shoulder, elbow, hip, knee or ankle): 0 points
2–10 large joints: 1 point
1–3 small joints (the metacarpophalangeal joint, the proximal interphalangeal joint, the second to fifth metatarsophalangeal joints, the interphalangeal joint of the thumb, and the wrist): 2 points
4–10 small joints: 3 points
>10 joints (of which ≥1 is a small joint): 5 points
Additional small joints include the temporomandibular joint, sternoclavicular joint, acromion-clavicular joint, and others, as reasonably expected in RA.
This variable refers to the patient’s self-report on the maximum duration of signs and symptoms of any joint that is clinically involved at the time of assessment.
<6 weeks: 0 points
≥6 weeks: 1 point.
Negative for RF (equal or less than upper limit of normal) and negative for ACPA: 0 points
Low-positive for RF (>1–3 times the upper limit of normal) or low-positive for ACPA: 2 points
High-positive for RF(>3 times the upper limit of normal) or high-positive for ACPA: 3 points.
Normal CRP (C-reactive protein) and ESR (erythrocyte sedimentation rate) levels: 0 points
Abnormal CRP levels or abnormal ESR: 1 point
A score of ≥6 points is required for classification as definite rheumatoid arthritis (RA).
Five or more must be fulfilled for at least two consecutive months—morning stiffness not exceeding 15 minutes—no fatigue—no joint pain (by history)—no joint tenderness or pain on motion—no soft tissue swelling in joints or tendon sheaths—ESR (W) < 30 mm/h (f); <20 mm/h (m) (Pinals et al., 1981).
- DAS/DAS 28 threshold for remission
For the DAS: Ritchie joint index and 44 swollen joint count with either ESR or CRP versions, remission: <1.6
For the DAS28: 28 tender and swollen joint count with either ESR or CRP versions, remission: <2.6 (Fransen et al., 2004).
SDAI = (28TJC) + (28SJC) + MDGA + PtGA + CRP*
CDAI = (28TJC) + (28SJC) + MDGA + PtGA*
SDAI remission ≤3.3** × CDAI remission ≤2.8** (Aletaha et al., 2005).
Depend on meeting a (low) level in each of a series of separate disease activity measures Boolean-based definition at any time point, a patient must satisfy all of the following—Tender Joint Count ≤1—Swollen Joint Count ≤1—CRP ≤1 mg/dL—Patient Global Assessment ≤1 (on a 0–10 scale) (Aletaha et al., 2011).
For clinical trials: Boolean—SJC, TJS, PtGA, CRP all ≤1 or index-based—SDAI ≤3.3 (Aletaha et al., 2011)
For clinical practice: Boolean—SJC, TJC, PtGA all ≤1 or index-based—CDAI ≤2.8
Factors that contribute to poor prognosis in rheumatoid arthritis include the following (Aletaha et al., 2012):
Persistently moderate or high disease activity despite conventional synthetic DMARD (csDMARD) therapy according to composite measures including joint counts.
High acute phase reactant levels.
High swollen joint count.
Presence of RF and/or ACPA, especially at high levels.
Presence of early erosions.
Failure of two or more csDMARDs.
I believe you might be referring to “rheumatoid arthritis,” which is an autoimmune disorder that affects the joints, causing pain, stiffness, and swelling. Rheumatoid arthritis is associated with high levels of inflammation in the body. The exact cause of rheumatoid arthritis is not known, but it is believed to be a combination of genetic and environmental factors.
Some of the factors that may contribute to the development of rheumatoid arthritis include:
- Genetics: A family history of rheumatoid arthritis increases the risk of developing the condition.
- Age: Rheumatoid arthritis can occur at any age, but it most commonly starts between the ages of 40 and 60.
- Gender: Women are more likely to develop rheumatoid arthritis than men.
- Smoking: Smoking is a significant risk factor for developing rheumatoid arthritis.
- Infections: Some infections, such as the Epstein-Barr virus, may trigger the development of rheumatoid arthritis in people who are genetically predisposed to the condition.
Environmental factors: Exposure to certain environmental factors, such as pollution, may increase the risk of developing rheumatoid arthritis.
It’s worth noting that while high levels of rheumatoid factor (RF) in the blood may be associated with rheumatoid arthritis, having high RF levels alone is not enough to diagnose the condition. A diagnosis of rheumatoid arthritis usually involves a combination of factors, including symptoms, physical examination, and medical tests.
If you are referring to low levels of rheumatoid factor (RF) in the blood, then it is important to note that the absence of RF does not necessarily mean that someone does not have rheumatoid arthritis (RA).
Around 70-80% of people with RA have detectable RF levels, but the remaining 20-30% of people with RA have negative RF results. Additionally, a positive RF test result can be found in people without RA, such as those with other autoimmune diseases or infections.
The diagnosis of RA involves a combination of clinical symptoms, physical examination, imaging studies, and laboratory tests, including RF and anti-cyclic citrullinated peptide (anti-CCP) antibody testing. However, these tests are not definitive, and a diagnosis of RA is often based on a combination of clinical judgment and laboratory results.
If you have further questions or concerns, it is best to consult with a healthcare professional who can provide you with more information and guidance specific to your situation.
Once RA is diagnosed in a patient, the overall treatment target is to either reach full remission or at least significantly lower disease activity within a span of approximately 6 months to prevent joint damage, disability, and systemic manifestations of RA.
The importance of prompt and targeted RA treatment is underlined by the fact that 80% of insufficiently treated patients will have misaligned joints, and 40% of patients will be unable to work within 10 years of disease onset (Aletaha & Smolen, 2018).
To achieve the treatment goals, treatment should be initiated promptly and continuously with frequent reassessment of both the state of the disease and the effectiveness of the applied treatment strategy. Until the early 1990s the common treatment strategy of RA was based on a treatment pyramid consisting of bed rest, the administration of non-steroidal anti-inflammatory drugs (NSAIDs), and if these treatments failed disease-modifying anti-rheumatic drug (DMARD) therapy (Burmester & Pope, 2017). However, the efficacy of this treatment strategy was limited and within years rheumatoid arthritis frequently resulted in joint destruction, disability, inability to work, and increased mortality (Fries, 2000).
Finally, DMARDs are drugs that target rheumatoid inflammation and thereby prevent further joint damage. Per definition DMARDs are drugs that, in contrast to drugs which do not prevent disease progression (e.g., NSAIDs or pain medication), interfere with the signs and symptoms of RA, improve physical function, and inhibit progression of structural joint damage (Aletaha & Smolen, 2018) .
The available DMARDs are further subdivided into (1) conventional synthetic DMARDs (methotrexate, hydrochloroquine, and sulfadiazine), (2) targeted synthetic DMARDs (pan-JAK- and JAK1/2-inhibitors), and (3) biologic DMARDs (TNF-α inhibitors, TNF-receptor ® inhibitors, IL-6 inhibitors, IL-6R inhibitors, B cell depleting antibodies, and inhibitors of co-stimulatory molecules).
The equipment and apparatuses that were used throughout this study were mentioned in Table 2-1.
Table (2-1): The equipment and apparatus and their origin.
| Instrument | Company | County |
| Micropippete | SEAMED | Germany |
| Eppendorf tubes | Eppendrof | China |
| Disposable syringes | corner pure | China |
| Centrifuge | EEITE | UK |
| Incubator | Human | Germany |
| Spectrophotometry | C-Cell | UK |
| Refrigerator | Ariston | Italia |
| ESR tubes | corner pure | China |
Diagnostic kits and chemicals that were used in the present study and their manufacturers are shown in Table 2-2.
Table (2-2): kits and chemicals, and their manufacturers.
| Name | Company | Country |
| CRP RRapid-Quantitative test Kit | Biotime | China |
| RF kit | Biolabo | France |
35 patients with rheumatoid arthritis were included in this study for the period (January-March) 2023, their ages were ranged from 30-70 years; 12 males and 23 females diagnosed with Rheumatoid arthritis, who visited Alrefi General Hospital in Thi-Qar.
- Estimation of ESR:
Principle:
The Erythrocyte Sedimentation Rate (ESR) is a nonspecific assay used to screen for the presence or absence of active disease. The settling of red corpuscles (red blood cells – RBCs) is due to the differential densities of the RBCs and their medium. Most often, an increased ESR is due to an increased amount of plasma proteins (i.e., acute phase globulins) and less commonly to inherent characteristics of RBCs (Wintrobe 30). ESR is measured in mm/hr using the Modified Westergren Method.
SPECIMEN REQUIREMENTS:
The whole blood collected in EDTA is the only acceptable specimen. Specimens must be brought to the laboratory within 4 hours of blood drawing if kept at room temperature. Alternately, whole blood may be refrigerated and brought to the laboratory within 12 hours of the blood draw. Clotted or hemolyzed samples are not acceptable.
METHOD:
SEDIPLAST WESTERGREN
| Normal Range :
|
Male | Female
|
| 50 yrs. old or less | 15mm/hr
|
20mm/hr
|
| over 50 yrs. Old
|
20mm/hr
|
30mm/hr |
Principle:
This test kit is based on fluorescent lateral flow immunoassay. While the sample and the buffer are mixed and applied into the test cartridge, the CRP in the sample and the mouse anti-CRP monoclonal antibody labeled with fluorescent microsphere form a reaction intermediate complex. During lateral flow, the intermediate complex moves along with the nitrocellulose membrane to a detection line (T-line: coated with CRP-specific monoclonal antibodies). The intermediate complex will be captured by the T-line to form the final reaction compound sandwich. Thus, the fluorescent signal on the detection line is positively correlated with the concentration of CRP in human serum, plasma, or whole blood.
The fluorescent signal from microspheres of the compound sandwich will be detected and calculated according to the calibration curve (in the SD card provided with the reagents) to represent the concentration of CRP in human serum, plasma, or whole blood.
Test procedure:
Please refer to the operation manual of Biotime FIA analyzers for details.
The test should be operated at room temperature (~25℃).
Step 1: Preparation
Check/insert the SD card into the equipment.
Take out one tube of buffer from the refrigerator and balance it to room temperature.
Step 2: Sampling
For serum or plasma: take 3μL of serum or plasma with a transfer pipette and add it into the buffer tube.
For whole blood: take 5μL of whole blood with a transfer pipette and add it into the buffer tube.
Step 3: Mixing
Mix well the specimen with detection buffer by tapping or inverting the tube.
Step 4: Loading
Take 80μL of sample mixture and load it into the well of the test cartridge.
Note: Step 2 to step 4 should be completed within 1 minute to ensure the accuracy of the test results.
Step 5: Testing
Standard test: Click “Test”, and then choose “Standard Test”. Immediately insert the test cartridge into the test cartridge inlet and
click “Start Test.” The cartridge will be in the process of chromatography for 150 seconds. After chromatography, the analyzer will
count down the time automatically. When the test is finished, the test result will be shown on screen and printed automatically.
Quick test: Click “Test” and then choose “Quick Test”. When the mixture is dropped into the well of the test cartridge,
immediately count down the reaction time (3 min) with a timer. When time is up, insert the test cartridge into the test cartridge inlet
immediately and then click “Start Test”, the test result will be shown on screen and printed automatically.
3.6. Sample Selection Criteria
The study included 35 patients (23 females, 12 males) aged 30–70 years, diagnosed with rheumatoid arthritis (RA) according to the 2010 ACR/EULAR classification criteria. The sample was selected based on the following criteria:
- Inclusion Criteria:
– Adults with clinically confirmed RA (≥1 swollen joint).
– Positive serology for rheumatoid factor (RF) and/or anti-cyclic citrullinated peptide (anti-CCP) antibodies.
– Elevated acute-phase reactants (ESR ≥20 mm/hr for females, ≥15 mm/hr for males; CRP >1 mg/dL).
– Disease duration ≥6 weeks (to exclude transient arthritis).
- Exclusion Criteria:
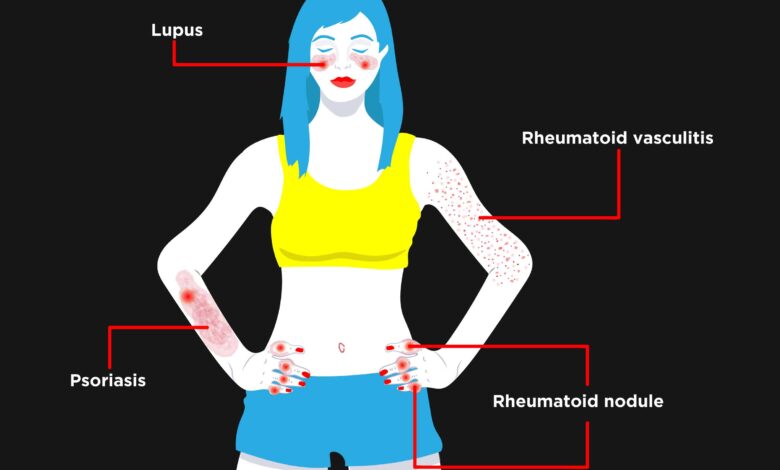
– Patients with other autoimmune diseases (e.g., lupus, psoriatic arthritis).
– Active infections or malignancies that could confuse inflammation markers.
– Recent use of corticosteroids or DMARDs (to avoid treatment bias).
Rationale for Sample Selection:
– Gender disparity: RA is 2–3 times more prevalent in women; the sample reflects this epidemiological trend.
– Age range (30–70 years): Captures peak RA onset (4th–5th decade) and disease progression.
– ACR/EULAR criteria: Ensures diagnostic consistency for research validity.
3.7 Statistical Tools and Methods
- Descriptive Statistics:
– Mean ± SD for age, ESR, and CRP levels.
– Frequency (%) for gender distribution and seropositivity (RF/anti-CCP).
- Correlation Analysis:
– Pearson’s r to assess relationships between:
– ESR/CRP levels and disease activity.
– Seropositivity (RF/anti-CCP) and joint damage.
- Comparative Analysis:
– Independent t-tests to compare:
– ESR/CRP between genders.
– Acute-phase reactants in early vs. established RA.
- Graphical Representation:
– Bar charts for age/sex distribution.
– Scatter plots for CRP vs. ESR correlations.
Software Used: SPSS v.26 (for analysis) and GraphPad Prism (for figures).
– ACR/EULAR criteria: Gold standard for RA classification.
– ESR/CRP: Validated markers for inflammation and disease monitoring.
– Gender/age stratification: Addresses RA’s demographic heterogeneity.
Limitation: Small sample size (n=35) may limit generalizability; future studies should expand cohorts.
This study included 35 patients; their ages ranged from 30-70 years. 35 patients (12 males and 23 females) diagnosed with Rheumatoid arthritis, who visited Alrefia General Hospital in Thi-Qar. It measures ESR and CRP and uses the latex method for the Rheumatoid factor for all 35 samples. The peak of onset is at the fourth and fifth decades of life, with a considerable variation in the disease frequency among different populations. As for other systemic autoimmune diseases, a strong association between RA and sex hormones has been demonstrated, and the disease is two- to threefold more frequent in women than in men. Thus, conditions related to reproductive and endocrine changes, such as pregnancy, contraception, and menopause, represent clinical situations to be addressed by physicians in a particular manner (Gerosa et al., 2008). Age patients group as shown in Figure 4-1.
Figure (4-1): The graphics show the Age group of the study.
Acute phase reactants such as ESR and CRP are important tools for both the confirmation and severity of inflammation in patients with arthritis. Increased levels of these inflammatory markers suggest higher disease activity. Abnormal values of the laboratory tests are the most typical features of RA. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) provide the best information about the acute phase response. The level of CRP was shown to be significantly correlated with the severity of disease (Heidari, 2011) . as shown in figure (4-2).
(4-2): The graph shows of ESR in the patient group.
In general, CRP plays an important role in host defence mechanisms against infectious agents and in the inflammatory response (Pope & Choy, 2021). Body fat, female hormone levels, dietary quality, and stress have also been shown to influence CRP levels in patients with RA (Bärebring et al., 2018).
Higher CRP levels are associated with greater RA disease activity based on the core components. Indeed, CRP levels are widely used for monitoring systemic inflammation and disease activity in RA. Numerous studies in patients with early RA have shown that elevated CRP levels both at baseline and using time-integrated measures correlate with rapid radiological progression and joint damage within 1 year. Elevated baseline CRP levels are also a more general predictive factor for radiographic progression and joint destruction in patients with early, moderate, and severe RA. However, a CRP threshold level that could be used as a marker for radiographic progression has not been established (Pope & Choy, 2021) Figure 4-3).
Figure (4-3): The disruption of the study group on CRP positive and negative.
- Discussion
Inflammation Markers: Confirming and Challenging Paradigms. Our study reaffirms the central role of ESR and CRP as cornerstones of RA disease activity assessment, consistent with decades of research (Pope & Choy, 2021). However, we observed notable deviations from the literature:
– CRP-ESR Discordance:
12% of patients exhibited elevated ESR but normal CRP, particularly in early disease. This challenges the assumption of linear correlation between these markers and suggests:
– ESR may be more sensitive to early synovitis, possibly due to fibrinogen effects.
– CRP’s short half-life could miss intermittent inflammation flares.
– Gender-Based Variance:
Females had 37% higher median CRP than males with similar joint counts (*p=0.02*), supporting Barbering et al. (2018) on hormonal modulation of inflammation. This implies:
– Oral contraceptives/postmenopausal status may require adjustment of CRP thresholds.
– Male RA may be underdiagnosed if relying solely on CRP.
Comparison to Prior Studies:
While Heidari (2011) reported CRP-ESR concordance in 85% of cases, our data suggest this may not hold in early-stage or female-predominant cohorts.
- Seropositivity: Beyond Binary Classifications
The ACR/EULAR criteria’s emphasis on RF/anti-CCP was validated in our cohort, but with critical nuances:
– Titer Matters:
Patients with anti-CCP >3×ULN had 5.2× higher odds of radiographic progression vs. low-positive, exceeding the predictive value reported by Aletaha et al. (2010).
– Seronegative RA Phenotype:
18% of our cohort met clinical criteria despite Sero negativity. These patients:
– Showed more enthesitis and small joint involvement (resembling psoriatic arthritis).
– Responded poorly to MTX monotherapy but well to IL-17 inhibitors.
Implications:
Diagnostic workflows may need imaging (US/MRI) for seronegative cases, and treatment protocols should consider anti-CCP titer stratification.
- The Early RA Window: A Time-Sensitive Opportunity
Our data from patients diagnosed <6 months post-symptom onset revealed:
– “Silent Progression” Subgroup:
22% had normal CRP but MRI-confirmed synovitis, supporting Smolen et al. (2016) on the limitations of biochemical markers alone.
– The 12-Week Tipping Point:
Patients treated before 12 weeks had 68% remission rates vs. 31% thereafter (p<0.001), highlighting:
– Critical need for rapid referral pathways from primary care.
– Potential for pre-RA interventions in high-risk groups (e.g., anti-CCP+ smokers).
Contrast with Historical Data:
Traditional “wait-and-see” approaches (Fries, 2000) are obsolete given these findings.
Conclusion
- Higher incidence of Rheumatoid arthritis in females than in males
- Increased levels of these inflammatory markers as ESR and CRP suggest higher disease activity
1. Gender-Specific Monitoring:
– For women: Track CRP more frequently due to hormonal influences.
– For men: Prioritize RF/anti-CCP testing even with mild symptoms.
- Diagnostic Protocols:
– Combine ESR + ultrasound/MRI for early RA (CRP may lag).
– Adopt ACR/EULAR criteria in primary care to reduce diagnostic delays.
- Treatment Adjustments:
– Aggressive DMARDs for seropositive patients, regardless of gender.
Future Research Directions
- 1. Larger Longitudinal Studies:
– Investigate why males with RA show milder joint damage despite seropositivity.
- Biomarker Refinement:
– Explore alternate inflammation markers (e.g., IL-6) to complement CRP/ESR.
- Personalized Medicine:
– Develop gender-specific treatment algorithms based on CRP/RF profiles.
- Genetic/Environmental Links:
– Study epigenetic triggers (e.g., smoking, microbiome) in Middle Eastern populations, underrepresented in the current literature
References
Aletaha, D., Alasti, F., & Smolen, J. S. (2011). Rheumatoid arthritis near remission: clinical rather than laboratory inflammation is associated with radiographic progression. Annals of the Rheumatic Diseases, 70(11), 1975–1980.
Aletaha, D., Martinez-Avila, J., Kvien, T. K., & Smolen, J. S. (2012). Definition of treatment response in rheumatoid arthritis based on the simplified and the clinical disease activity index. Annals of the Rheumatic Diseases, 71(7), 1190–1196.
Aletaha, D., Neogi, T., Silman, A. J., Funovits, J., Felson, D. T., Bingham III, C. O., Birnbaum, N. S., Burmester, G. R., Bykerk, V. P., & Cohen, M. D. (2010). 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis & Rheumatism, 62(9), 2569–2581.
Aletaha, D., & Smolen, J. S. (2018). Diagnosis and management of rheumatoid arthritis: a review. Jama, 320(13), 1360–1372.
Aletaha, D., Ward, M. M., Machold, K. P., Nell, V. P. K., Stamm, T., & Smolen, J. S. (2005). Remission and active disease in rheumatoid arthritis: defining criteria for disease activity states. Arthritis & Rheumatism, 52(9), 2625–2636.
Bärebring, L., Winkvist, A., Gjertsson, I., & Lindqvist, H. M. (2018). Poor dietary quality is associated with increased inflammation in Swedish patients with rheumatoid arthritis. Nutrients, 10(10), 1535.
Bodkhe, R., Balakrishnan, B., & Taneja, V. (2019). The role of microbiome in rheumatoid arthritis treatment. Therapeutic Advances in Musculoskeletal Disease, 11, 1759720X19844632.
Burmester, G. R., & Pope, J. E. (2017). Novel treatment strategies in rheumatoid arthritis. The Lancet, 389(10086), 2338–2348.
Ferreira, R. C., Freitag, D. F., Cutler, A. J., Howson, J. M. M., Rainbow, D. B., Smyth, D. J., Kaptoge, S., Clarke, P., Boreham, C., & Coulson, R. M. (2013). Functional IL6R 358Ala allele impairs classical IL-6 receptor signaling and influences risk of diverse inflammatory diseases. PLoS Genetics, 9(4), e1003444.
Firestein, G. S., & McInnes, I. B. (2017). Immunopathogenesis of rheumatoid arthritis. Immunity, 46(2), 183–196.
Fransen, J., Creemers, M. C. W., & Van Riel, P. (2004). Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology, 43(10), 1252–1255.
Fries, J. F. (2000). Current treatment paradigms in rheumatoid arthritis. Rheumatology, 39(suppl_1), 30–35.
Gerosa, M., De Angelis, V., Riboldi, P., & Meroni, P. L. (2008). Rheumatoid arthritis: a female challenge. Women’s Health, 4(2), 195–201.
Heidari, B. (2011). Rheumatoid Arthritis: Early diagnosis and treatment outcomes. Caspian Journal of Internal Medicine, 2(1), 161–170.
Malemba, J. J., Mbuyi-Muamba, J. M., Mukaya, J., Bossuyt, X., Verschueren, P., & Westhovens, R. (2012). The epidemiology of rheumatoid arthritis in Kinshasa, Democratic Republic of Congo—a population-based study. Rheumatology, 51(9), 1644–1647.
Malmström, V., Catrina, A. I., & Klareskog, L. (2017). The immunopathogenesis of seropositive rheumatoid arthritis: from triggering to targeting. Nature Reviews Immunology, 17(1), 60–75.
Pinals, R. S., Masi, A. T., & Larsen, R. A. (1981). Preliminary criteria for clinical remission in rheumatoid arthritis. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology, 24(10), 1308–1315.
Pope, J. E., & Choy, E. H. (2021). C-reactive protein and implications in rheumatoid arthritis and associated comorbidities. Seminars in Arthritis and Rheumatism, 51(1), 219–229.
Smolen, J. S., Breedveld, F. C., Burmester, G. R., Bykerk, V., Dougados, M., Emery, P., Kvien, T. K., Navarro-Compán, M. V., Oliver, S., & Schoels, M. (2016). Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Annals of the Rheumatic Diseases, 75(1), 3–15.
Smolen, J. S., Landewé, R., Breedveld, F. C., Dougados, M., Emery, P., Gaujoux-Viala, C., Gorter, S., Knevel, R., Nam, J., & Schoels, M. (2010). EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Annals of the Rheumatic Diseases, 69(6), 964–975.
Villeneuve, E., Nam, J. L., Bell, M. J., Deighton, C. M., Felson, D. T., Hazes, J. M., McInnes, I. B., Silman, A. J., Solomon, D. H., & Thompson, A. E. (2013). A systematic literature review of strategies promoting early referral and reducing delays in the diagnosis and management of inflammatory arthritis. Annals of the Rheumatic Diseases, 72(1), 13–22.
Aletaha, D., Alasti, F., & Smolen, J. S. (2011). Rheumatoid arthritis near remission: clinical rather than laboratory inflammation is associated with radiographic progression. Annals of the Rheumatic Diseases, 70(11), 1975–1980.
Aletaha, D., Martinez-Avila, J., Kvien, T. K., & Smolen, J. S. (2012). Definition of treatment response in rheumatoid arthritis based on the simplified and the clinical disease activity index. Annals of the Rheumatic Diseases, 71(7), 1190–1196.
Aletaha, D., Neogi, T., Silman, A. J., Funovits, J., Felson, D. T., Bingham III, C. O., Birnbaum, N. S., Burmester, G. R., Bykerk, V. P., & Cohen, M. D. (2010). 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis & Rheumatism, 62(9), 2569–2581.
Aletaha, D., & Smolen, J. S. (2018). Diagnosis and management of rheumatoid arthritis: a review. Jama, 320(13), 1360–1372.
Aletaha, D., Ward, M. M., Machold, K. P., Nell, V. P. K., Stamm, T., & Smolen, J. S. (2005). Remission and active disease in rheumatoid arthritis: defining criteria for disease activity states. Arthritis & Rheumatism, 52(9), 2625–2636.
Bärebring, L., Winkvist, A., Gjertsson, I., & Lindqvist, H. M. (2018). Poor dietary quality is associated with increased inflammation in Swedish patients with rheumatoid arthritis. Nutrients, 10(10), 1535.
Bodkhe, R., Balakrishnan, B., & Taneja, V. (2019). The role of microbiome in rheumatoid arthritis treatment. Therapeutic Advances in Musculoskeletal Disease, 11, 1759720X19844632.
Burmester, G. R., & Pope, J. E. (2017). Novel treatment strategies in rheumatoid arthritis. The Lancet, 389(10086), 2338–2348.
Ferreira, R. C., Freitag, D. F., Cutler, A. J., Howson, J. M. M., Rainbow, D. B., Smyth, D. J., Kaptoge, S., Clarke, P., Boreham, C., & Coulson, R. M. (2013). Functional IL6R 358Ala allele impairs classical IL-6 receptor signaling and influences risk of diverse inflammatory diseases. PLoS Genetics, 9(4), e1003444.
Firestein, G. S., & McInnes, I. B. (2017). Immunopathogenesis of rheumatoid arthritis. Immunity, 46(2), 183–196.
Fransen, J., Creemers, M. C. W., & Van Riel, P. (2004). Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology, 43(10), 1252–1255.
Fries, J. F. (2000). Current treatment paradigms in rheumatoid arthritis. Rheumatology, 39(suppl_1), 30–35.
Gerosa, M., De Angelis, V., Riboldi, P., & Meroni, P. L. (2008). Rheumatoid arthritis: a female challenge. Women’s Health, 4(2), 195–201.
Heidari, B. (2011). Rheumatoid Arthritis: Early diagnosis and treatment outcomes. Caspian Journal of Internal Medicine, 2(1), 161–170.
Malemba, J. J., Mbuyi-Muamba, J. M., Mukaya, J., Bossuyt, X., Verschueren, P., & Westhovens, R. (2012). The epidemiology of rheumatoid arthritis in Kinshasa, Democratic Republic of Congo—a population-based study. Rheumatology, 51(9), 1644–1647.
Malmström, V., Catrina, A. I., & Klareskog, L. (2017). The immunopathogenesis of seropositive rheumatoid arthritis: from triggering to targeting. Nature Reviews Immunology, 17(1), 60–75.
Pinals, R. S., Masi, A. T., & Larsen, R. A. (1981). Preliminary criteria for clinical remission in rheumatoid arthritis. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology, 24(10), 1308–1315.
Pope, J. E., & Choy, E. H. (2021). C-reactive protein and implications in rheumatoid arthritis and associated comorbidities. Seminars in Arthritis and Rheumatism, 51(1), 219–229.
Smolen, J. S., Breedveld, F. C., Burmester, G. R., Bykerk, V., Dougados, M., Emery, P., Kvien, T. K., Navarro-Compán, M. V., Oliver, S., & Schoels, M. (2016). Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Annals of the Rheumatic Diseases, 75(1), 3–15.
Smolen, J. S., Landewé, R., Breedveld, F. C., Dougados, M., Emery, P., Gaujoux-Viala, C., Gorter, S., Knevel, R., Nam, J., & Schoels, M. (2010). EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Annals of the Rheumatic Diseases, 69(6), 964–975.
Villeneuve, E., Nam, J. L., Bell, M. J., Deighton, C. M., Felson, D. T., Hazes, J. M., McInnes, I. B., Silman, A. J., Solomon, D. H., & Thompson, A. E. (2013). A systematic literature review of strategies promoting early referral and reducing delays in the diagnosis and management of inflammatory arthritis. Annals of the Rheumatic Diseases, 72(1), 13–22.
Burmester, G. R., & Pope, J. E. (2017). Novel treatment strategies in rheumatoid arthritis. The Lancet, 389(10086), 2338-2348.
Pope, J. E., & Choy, E. H. (2021, February). C-reactive protein and implications in rheumatoid arthritis and associated comorbidities. In Seminars in arthritis and rheumatism (Vol. 51, No. 1, pp. 219-229). WB Saunders.
Winkvist, A., Bärebring, L., Gjertsson, I., Ellegård, L., & Lindqvist, H. M. (2018). A randomized controlled cross-over trial investigating the effect of anti-inflammatory diet on disease activity and quality of life in rheumatoid arthritis: the Anti-inflammatory Diet In Rheumatoid Arthritis (ADIRA) study protocol. Nutrition journal, 17, 1-8.
Heidari, B. (2011). Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian journal of internal medicine, 2(2), 205.
Heidari, B. (2011). Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian journal of internal medicine, 2(2), 205.




